I think this sort of debate runs together two separate questions:
(1) Is the neurophysiology upon which pain-involving mental states supervene present in fetuses of x weeks?
and
(2) Is fetal pain --if it exists-- bad for the fetus?
Here's two reasons for thinking they come apart.
First, it's worth remembering that the aversiveness of pain is to some extent learned (see, for example, the famous McGill dog study). It might be that there is a pain sensation, but that the fetus has not learned to experience it as something bad. There might be evidence for or against this. But it probably wouldn't come from the fetus exhibiting near-reflex escape behaviors. IIRC, in adults many such behaviors are triggered very early in pain processing, even before much of the emotional processing occurs.
Second, there's the very hard question of whether fetuses are yet the sort of creatures that can have things be bad for them. Though I'm obsessed with the general problem (what makes something the subject of agent-relative value) I won't even try to articulate this one here. Especially because it actually a complex of several different super-hard issues.
Omaha.com - The Omaha World-Herald: Metro/Region - When can fetus feel pain?: "Knowing when a fetus first feels pain is like many scientific endeavors: It involves speculation and disagreement.
A bill before the Nebraska Legislature, the Abortion Pain Prevention Act, would ban abortions 20 weeks after conception, because it's at that point, Speaker of the Legislature Mike Flood says, that a fetus begins to sense pain.
‘The science is compelling,’ the Norfolk lawmaker wrote on his Web site about the bill that is scheduled for a hearing Feb. 25.
In fact, there still is considerable disagreement among scientists, physicians and other experts. It's fairly common for a person's position on the question to mirror his position on abortion. But it's not clear when the complex communication circuitry in the body, spine and brain are developed enough for pain to be felt.
Nerve fibers designed to sense pain are present in a fetus's skin seven or eight weeks after conception, said Dr. Terence Zach, chairman of pediatrics at the Creighton University School of Medicine.
Surely by 20 weeks, Zach said, a fetus is mature enough to respond to what scientists call ‘noxious stimuli,’ or pain.
‘I believe that — yep,’ said Zach, who described himself as pro-life.
Another Omaha physician, Dr. Robert Bonebrake, agrees with Zach. Bonebrake, a perinatologist at Methodist Hospital, sometimes must give blood transfusions to fetuses or drain fluid from them at 21 or 22 weeks.
Those procedures involve inserting a needle or shunt into the fetus. Bonebrake said the fetus will ‘back away a little bit’ from the needle, indicating to him that it has felt the jab.
‘He or she will try to move away if possible,’ said Bonebrake, who also described himself as pro-life.
But in a review of fetal pain literature, University of California-San Francisco physicians reported in 2005 that ‘fetal perception of pain is unlikely before the third trimester,’ or about 27 weeks into the pregnancy.
The review, published in the Journal of the American Medical Association, said reflex movement isn't proof of pain, because it can occur without the brain being developed enough for conscious pain recognition.
The article also stated that only 1.4 percent of abortions in the U.S. occur at or after 21 weeks.
In Nebraska, fetal age doesn't have to be reported and usually isn't, according to a state health spokeswoman. But in cases where it was reported, none of the abortions that occurred in Nebraska in 2008 involved fetuses of 20 weeks or older.
The American College of Obstetricians and Gynecologists' position is that it ‘knows of no legitimate scientific information that supports the statement that a fetus experiences pain at 20 weeks' gestation.’
A Children's Hospital Boston anesthesiologist and researcher, Dr. Roland Brusseau, has studied the subject to determine whether a fetus undergoing a surgical procedure should have anesthesia. His institution is the main children's hospital of Harvard Medical School.
Brusseau calls discussions of fetal pain ‘complicated and controversial.’
He has suggested a broad timeline for when fetal pain might start: ‘If we are to accept that consciousness is possible by 20 weeks (or more conservatively, 30 weeks), then it also would appear possible that fetuses could experience something approximating ‘pain,'’ he wrote a little more than three years ago.
The possibility, he said, would appear to mandate the use of appropriate anesthesia when performing fetal surgery.
Federal legislation has been unsuccessfully introduced over the past several years to require abortion providers to inform the mother that the fetus could feel pain at 20 weeks and offer anesthesia directly to the fetus.
Six states — Oklahoma, Arkansas, Utah, Georgia, Louisiana and Minnesota — have passed similar legislation, according to the Center for Reproductive Rights in New York.
In Iowa, a bill to that effect in the Legislature failed in 2005.
What makes Flood's legislation different is that its answer to the question of fetal pain is to ban abortions after 20 weeks. Exceptions would be allowed if an abortion is deemed necessary to avoid substantial harm or death to the mother.
Flood said that laws protect animals in slaughterhouses from excessive pain, and that fetuses deserve that level of sensitivity.
He said he based his beliefs that fetuses feel pain at 20 weeks in part on assertions by Drs. Jean Wright and K.J.S. ‘Sunny’ Anand. Wright is former chairwoman of pediatrics at Mercer University School of Medicine's Savannah, Ga., campus and Anand is chief of pediatric critical care at the University of Tennessee Health Science Center.
Flood said experts have found, for instance, that stress hormones spike when fetuses undergo invasive procedures.
Wright couldn't be reached for comment, but Anand, who was reached while doing humanitarian work in Haiti, said fetuses show signs of sensory perception around 20 weeks.
‘Whether this happens at 20 weeks or 22 weeks or 18 weeks is still open to question,’ Anand said. Some fetuses might develop more quickly than others, he said.
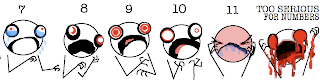
Anand said he believes the sense of pain in a fetus isn't turned on like a light switch. ‘It's more like a dimmer switch that very slowly — very, very gradually — turns on particular sensory modalities.’
Anand said the chain of connections for pain perception includes nerve fibers, spinal cord circuitry, brain stem and other portions of the brain. It's impossible to know for sure whether a fetus feels pain, he said.
But denying there is pain, he said, means there's no incentive to study it, no reason to work out ways to anesthetize fetuses, and no need for a doctor to consider whether pain is being inflicted.
‘But I think the onus is on us to give the benefit of the doubt,’ he said.
Anand said he believes abortion is appropriate in some instances, such as if a teenager has been raped, and inappropriate in others, such as when a woman has broken up with a boyfriend and then learns she's pregnant.
Arthur Caplan, professor of medical ethics and director of the Center for Bioethics at the University of Pennsylvania, said that ‘on the whole, I don't think science and medicine can be drawn in to support’ Flood's bill.
Caplan, who has a doctorate in philosophy, called himself ‘a conservative pro-choicer.’ He said that there is no consensus among physicians and scientists on the subject of fetal pain and that the notion that pain is felt at 20 weeks is ‘not the mainstream opinion.’
Bellevue abortion provider Dr. LeRoy Carhart, who has said he will perform late-term abortions only in cases when the fetus can't survive outside the womb, said he doesn't believe there is fetal pain before or during his abortions.
Nevertheless, Carhart said when performing abortions in cases where the fetus is 17 weeks or older, he sedates the mother — which sedates the fetus — and then administers another injection to stop the fetus's heart. The abortion typically occurs 24 to 72 hours later, he said.
‘This should be the ‘Put Carhart Out of Business Bill,'’ he said of Legislative Bill 1103.
Flood denied that his bill was directed at Carhart's revenue and said: ‘Dr. Carhart's loss of business pales in comparison to the loss of young lives.’
Dr. Michael Barsoom, director of maternal-fetal medicine at the Creighton School of Medicine, said he has seen fetuses move away from needles when needles are put in or near them.
Whether that's a reaction to pain, though, is unclear, Barsoom said. The fetus might respond reflexively and not as a conscious pain experience, he said.
‘I honestly don't know,’ said Barsoom, who described himself as pro-life. He said he doesn't think anyone can say for sure when a fetus begins to feel pain.
‘I don't think there's any way to find out.’"